Clinical Trial
Higher CO2 Levels Have a Concerning Effect on Viruses Floating Through The Air

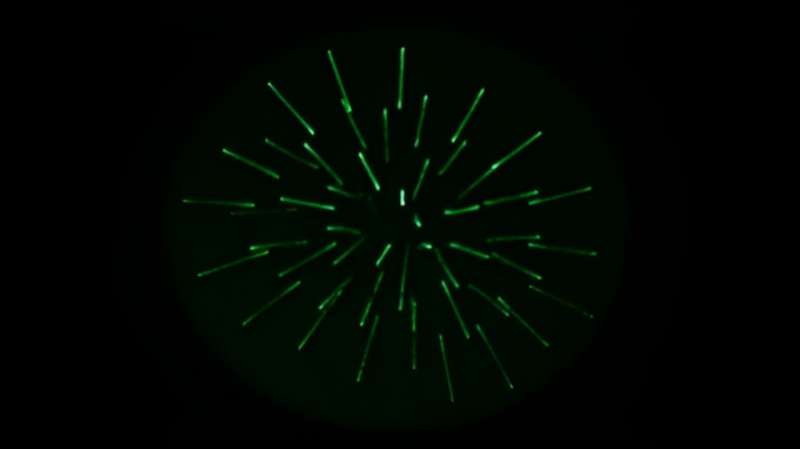
Virus containing droplets were suspended in the CELEBS experimental device for different durations before infectivity was tested. (Allen Haddrell/University of Bristol)
Keeping CO2 levels low reduces infectious airborne viral loads, new research suggests. While the study focused on the pathogen behind COVID-19, it has clear implications for reducing the risk of transmitting viruses in spaces where ventilation is limited.
“Opening a window may be more powerful than originally thought,” says University of Bristol chemist Allen Haddrell, “especially in crowded and poorly ventilated rooms, as fresh air will have a lower concentration of CO2, causing the virus to become inactivated much faster.”
By measuring SARS-CoV-2 capacity to remain infectious while aerosolized in droplets under different environmental conditions, Haddrell and colleagues discovered the virus’s stability is directly impacted by CO2levels in the air. They used a new technique called Controlled Electrodynamic Levitation and Extraction of Bioaerosol onto a Substrate (CELEBS), which measures the impact of temperature, relative humidity, and different gas concentrations on suspended virus particles.
Atmospheric CO2 concentrations are currently around 400 parts per million (ppm). Crowd enough people in a closed room, however, concentrations can soar to around 3,000 ppm. The team found the number of viral particles that can remain infectious under these elevated concentrations can be 10 times higher than what would be found in outdoor air.
“The high pH of exhaled droplets containing the SARS-CoV-2 virus is likely a major driver of the loss of infectiousness,” explains Haddrell. “CO2 behaves as an acid when it interacts with droplets. This causes the pH of the droplets to become less alkaline, resulting in the virus within them being inactivated at a slower rate.”
What’s more, highly crowded environments in poorly ventilated spaces can exceed 5,000 ppm of CO2.
“This relationship sheds important light on why super spreader events may occur under certain conditions,” notes Haddrell.
Interestingly, different strains of SARS-CoV-2 had different patterns of stability in the air. After only 5 minutes viable viral particle concentrations were 1.7 times higher for Omicron (BA.2) than for Delta. This suggests there may be a lot of variability between viral particle types.
So while more research is required to confirm the relationships between CO2 and other types of viruses, the researchers suspect this could explain why many respiratory viruses have seasonality. During colder weather people are likely to spend more time indoors experiencing greater exposure to air with higher levels of CO2.
The amount of CO2 in our outdoor air is also increasing thanks to global warming. Recent projections predict concentrations could exceed 700 ppm by the end of the century.
“[This study] also highlights the importance of our global net zero goals because the research indicates even slightly raised levels of CO2 , which are increasing in the atmosphere with the onset of climate change, can significantly improve the rate of virus survival and the risk of it spreading,” Haddrell adds.
“These findings can serve as a scientific basis for the design of mitigation strategies that could save lives in any future pandemic,” concludes University of Bristol physical chemist Jonathan Reid.
This research was published in Nature Communications.
Source : 1
Ayush and herbal products exports register 3.6% growth in 2023-24
| India’s export of Ayush and herbal products has reported a growth of 3.6 per cent during the fiscal year 2023-24, at $651.17 million as compared to the same period of previous year, registering a below-five per cent growth for the second consecutive year. The country reported exports of 10.63 crore kilograms of Ayush and herbal products during 2023-24, as compared to 12.25 crore kilograms of exports during the previous year. In terms of value, it has gone up from $628.54 million in 2022-23, according to data from the Directorate General of Commercial Intelligence and Statistics (DGCI&S). The year 2022-23 registered a growth of 2.68 per cent in exports, from $612.12 million in the previous year. The country has seen exports shooting up in two years during the fiscal years 2020-21 and 2021-22, before reporting a lower growth rate, according to official data. During 2020-21, the sector registered a growth of 26.12 per cent growth in exports, to $539.88 million from $428.08 million exports reported during the previous year. The exports then reported a growth of 13.38 per cent in 2021-22, at $612.12 million, says data from the Centre. It may be noted that the growth in terms of exports also were the years when the world went through the Covid-19 pandemic. The Ministry of Ayush has earlier claimed that the consumption of Ayush products, especially for health and wellness, has gone up during the time of the pandemic. The government also took initiatives to promote the systems of medicine with emphasis on its impact on improving the immunity and health of the users. The total Ayush export of India is around $1.54 billion (Rs. 11,400 crore), said the Ministry of Ayush in its recent report on the progress of the sector from 2014-2024. Presently, Ayurveda is recognized as a system of Traditional Medicine in more than 30 countries and Ayush and Herbal products or medicines are exported to more than 150 countries, says. The herbal pharmaceutical or medicament sector constituted 35.2% of Ayush exports in 2020, while the extracts and nutraceuticals sector shared around 22% export share each in the total, whereas medicinal and aromatic plant recorded 19.9% export share, said Invest India, the National Investment Promotion and Facilitation Agency. India exports Ayush products to markets such as the USA, Nepal, Russia, Philippines, UAE, Kenya, Germany, Vietnam, China, Italy, the UK, Western Europe, Japan, Hong Kong etc,. The Ayush sector has grown 17% year on year between 2014 and 2020. The market size of the industry stands at $18.1 billion from $2.85 billion in 2014, clocking a phenomenal growth of almost 6 times. The sector is likely to generate nearly 3 million job opportunities, it said. Share of sub-sectors in Ayush market size are herbal plants (43.35%), nutraceuticals (24.65%), pharmaceuticals (14.11%), cosmeceuticals (8.37%), plant derivatives (5.14%) and plant extracts (4.39%). The sector of herbal medicine grew at the rate of 7.4 % per annum during 2014-20. Various sub-sectors, particularly, the herbal pharmaceutical sector expanded at the rate of 18.5 % during the same period with the market share of 14.1 % in 2020, added the agency. The Ministry of Ayush has established Ayush Export Promotion Council (AYUSHEXCIL) to promote Ayush products and services globally by the Ministry of Ayush and supported by the Union Ministry of Commerce. It was officially launched at Global Ayush Investment and Innovation Summit held in Gandhinagar, Gujarat on April 20, 2022, and aimed to oversee exports of products of Ayurveda, Homoeopathy, Siddha, Sowa/Rigpa and Unani systems and address trade issues pertaining to these sectors. Ayush & Herbal Products Exports Year Exports (in US$ mn) Growth Rate (%) 2019-20 428.08 4.46 2020-21 539.88 26.12 2021-22 612.12 13.38 2022-23 628.54 2.68 2023-24 651.17 3.6 Sources: DGCI&S, Rajya Sabha |
Scientists Discover a Missing Link Between Diet And Cancer Risk

A previously unknown mechanism for inactivating genes that suppresses tumor formation helps explain why cancer risk is associated with an unhealthy diet or unmanaged metabolic conditions like diabetes.
Researchers from Singapore and the UK used mouse models, human tissue, and human breast organoids grown in the lab to find that changes in glucose metabolism could help cancer grow by temporarily disabling a gene that protects us from tumors called BRCA2.
“These findings raise awareness of the impact of diet and weight control in the management of cancer risks,” says the first author of the new study, cancer pharmacologist Li Ren Kong from the Cancer Science Institute of Singapore (CSI Singapore).
“We started the study aiming to understand what factors elevate risk in families susceptible to cancer, but ended up discovering a deeper mechanism linking an essential energy consumption pathway to cancer development.”
The discovery also challenges a long-established theory about genes that protect against cancer. Knudson’s ‘two-hit’ paradigm, first proposed in 1971, states that both copies of a tumor suppressor gene must be permanently inactivated in our cells before cancer can start.
Recent studies found that a mutation in one of a cell’s two BRCA2 genes is implicated in various cancers. Interestingly, mice and human cells with this mutation don’t show the usual signs of genetic instability seen in cells with both copies of the gene mutated.
In mice, having just one copy of BRCA2 affected doesn’t seem to cause major issues in organ development or DNA repair in most tissues. But cells with this mutation appear more vulnerable to stresses, like exposure to environmental toxins such as formaldehyde or acetaldehyde, which can reduce their levels of BRCA2 protein, leading to functional problems.
“How such environmental factors increase cancer risk is not yet very clear, but it is vital to understand the connection if we are to take preventive measures that help us stay healthy longer,” says oncologist and cancer researcher Ashok Venkitaraman from CSI Singapore.
The team first examined people who inherited one faulty copy of BRCA2. They found that cells from these people were more sensitive to methylglyoxal (MGO), which is produced when cells break down glucose for energy in the process of glycolysis.
Glycolysis generates over 90 percent of the MGO in cells, which a pair of enzymes typically keep to minimal levels. In the event they can’t keep up, high MGO levels can lead to the formation of harmful compounds that damage DNA and proteins. In conditions like diabetes, where MGO levels are elevated due to high blood sugar, these harmful compounds contribute to disease complications.
The researchers discovered that MGO can temporarily disable the tumor-suppressing functions of the BRCA2 protein, resulting in mutations linked to cancer development. This effect could be seen in noncancerous cells as well as patient-derived tissue samples, in some cases of human breast cancer, and in mouse models of pancreatic cancer.
As the BRCA2 allele isn’t permanently inactivated, functional forms of the protein it produces can later return to normal levels. But cells repeatedly exposed to MGO may continue to accumulate cancer-causing mutations whenever existing BRCA2 protein production fails.
Overall, this suggests that changes in glucose metabolism can disrupt BRCA2 function via MGO, contributing to the development and progression of cancer.
These results come from lab tests and small human tissue sample sizes, and the researchers say more studies need to be done using larger clinical studies or animal models to look into possible links between dietary factors, diabetes, and other metabolic disorders.
As MGO can temporarily rob the BRCA2 protein of its ability to repair DNA, it makes sense that a poor diet or uncontrolled diabetes could contribute to a higher risk of cancer over time, even in people with two functional copies of the BRCA2 gene. This new information may lead to strategies for cancer prevention or early detection.
“Methylglyoxal can be easily detected by a blood test for HbA1C, which could potentially be used as a marker,” Venkitaraman says.
“Furthermore, high methylglyoxal levels can usually be controlled with medicines and a good diet, creating avenues for proactive measures against the initiation of cancer.”
The research has been published in Cell.
Source : 1
Indian medical care providers explore HCX platforms to reduce administrative tasks in insurance claims
Indian medical care providers are exploring Health Exchange (HCX) platforms for reducing administrative tasks in insurance claims. It maximises cloud computing, allowing access in real-time, and secure information related to insurance claims. It enables seamless interoperability of health claim data between different systems, whilst safeguarding sensitive medical information at all costs.
Gaurav Gupta, co-founder & CEO, CarePay said, India follows a decentralized approach when it comes to the penetration of health insurance as merely 37% of its population are covered under the present schemes while nearly 400 million have zero access to health insurance.
Amidst the growing discrepancies in the decentralized healthcare insurance industry which is plagued by non-digitised and non-standardised processes, the interlude of the health claims exchange platform represents a revolution in healthcare. Moving beyond merely being another digital lending platform, HCX is a community-driven initiative in alignment with the government’s Ayushman Bharat Digital Mission, aiming to offer universal health coverage via the aid of HCX data exchange, he added.
HCX acts as a platform geared to transform the management of health insurance claims with efficiency.
With digitisation, HCX opens doors to electronic health records, which at the disposal of healthcare professionals enable them to access a patient’s comprehensive information, including insurance coverage and other essential details. Along with a seamless flow of data exchange amongst multiple systems, it improves patient experience, whilst mitigating the possibility of any discrepancies, Gupta a told Pharmabiz in an email.
Further, HCX expedites the settlement process from pre-authorization to discharge which lowers associated expenses. Simultaneously, it enables accessibility as nearly 6 out of 10 patients don’t have enough monetary capacity or insurance coverage.
Being a digital claims platform, it brings together multiple stakeholders under one unified pool, from policyholders to healthcare providers. Primarily, policyholders will get real-time updates of the claim through a simplified flow of information.
Gupta noted that it is already certain an efficient and transparent insurance claim process fosters better decision-making for individuals who pay for that policy. Besides, reduced overhead costs empower healthcare providers to focus from administrative tasks and capitalize on delivering enhanced patient care.
HCX data provides information on the borrower’s spending habits, enabling lenders to have a more holistic view of the person’s financial responsibility. It also helps FinTech and lending startups in making better credit decisions. With assessment algorithms, it opens financial access to the underserved segment of the population, he said.
Individuals can analyze their HCX data and streamline their spending making room for improved budgeting, debt reduction, and get the financial security. It helps them to look for loan options that are tailored best to their financial needs. Therefore, a Health Exchange develops a standardized health insurance framework with refined the settlement process from pre-authorization to discharge. Apart from building an open community amongst policyholders, payers, stakeholders, healthcare providers and other involved entities, the platform is focused on improving the insurance experience with informed decision-making, said Gupta.
Source : 1
A Healthy Lifestyle Could Offset Genetic Risk For Early Death by a Hopeful 62%

When research tells us that our grandparents’ diets can affect our health decades later, it can be hard to shake the feeling that genetics spells out the trajectory of our wellbeing.
But how much of our health is actually determined by our genes, and what effect does our lifestyle have, for better or worse? Can we really overcome the genetic cards we’ve been dealt and extend our lives by eating well and exercising often, as some research suggests?
A new study of more than 350,000 people from the UK has found that healthy lifestyle choices could offset the genetic risk of dying young by as much as 62 percent.
“To our knowledge, our study is the first to investigate the joint association of genetic risk and lifestyle factors with human lifespan,” the researchers write in their published paper.
Previous epidemiological studies have looked at one or the other, but with data from three large, long-term population studies investigating the links between genetics, environment, and disease, this new study could compare the effect of genetic risk and lifestyle factors on longevity simultaneously.
The team of researchers from several universities in China and the University of Edinburgh in the UK analyzed data on more than 350,000 adults of European descent, who were recruited to the UK Biobank study from 2006 to 2010, and followed for a median of almost 13 years.
The participants were asked about their diet, physical activity, smoking, alcohol intake, body shape, and sleep duration, and grouped into three tiers based on their responses. The researchers also split participants into three categories based on known genetic risk factors called polygenic risk scores – drawn from US studies – affecting lifespan.
Similar to previous family studies, the researchers found that genetics alone can raise the risk of early death by 21 percent.
An unhealthy lifestyle featuring poor sleep, little exercise, processed food, cigarettes, and alcohol was also linked to a 78 percent greater risk of dying early, regardless of someone’s genetic predisposition.
People with an unhealthy lifestyle and a genetic predisposition to a shorter lifespan were twice as likely to die from non-accidental, non-COVID related conditions during the study period as those with a lower genetic risk and more favorable lifestyle habits.
But opting for a healthier lifestyle – mainly by not smoking, exercising regularly, eating well and getting enough sleep – offset the genetic risk of a shorter life by 62 percent, the researchers found.
“This study elucidates the pivotal role of a healthy lifestyle in mitigating the impact of genetic factors on lifespan reduction,” the researchers conclude.
This is an observational study, however, so no firm conclusions can be drawn about cause and effect. Most of the participants were of white-European ancestry, so the findings can’t be generalized to other populations either.
What’s more, participants were surveyed about their lifestyle at only one point in time, when they joined the study, and the genetic variants studied captured only a small fraction of the genetic risk associated with a shorter lifespan, so there could be much more DNA in play.
Another big question this study touched on only briefly is at what age people make positive changes to their lifestyles.
The analysis found that people with a high genetic risk of a shorter life could add roughly another 5 years to their life expectancy at age 40 if they had implemented lifestyle changes. Other research shows the importance of maintaining them.
“Given that lifestyle behavioral habits are usually developed before middle age, taking effective public health interventions is quite crucial for those at high genetic risk to extend their lifespan before the formation of a fixed lifestyle,” the researchers conclude.
The study has been published in BMJ Evidence-Based Medicine.
Source : 1